Skin Cancer
What is Skin Cancer?

Skin cancer is a disease in which malignant (cancer) cells form in the tissues of the skin. Skin cancer is the only cancer that can be seen on the surface of the skin. These cancers are very curable if found early. By examining your skin for any changes, you can detect early warning signs of skin cancer. At Forefront Dermatology, formerly Asarch Dermatology, we treat skin cancers of varying types and urge our patients to check their skin frequently for changes.
Our practice values each and every patient. Our team of medical experts received specialized training in their respective fields to provide our patients with the most up to date treatments, procedures and the highest standard of care.
Who Is LIKELY tO GET SKIN CANCER?
Anyone can get skin cancer. Sun and indoor tanning are the leading causes of skin cancer.
The most likely people to get skin cancer:
- Spend a lot of time in the sun.
- Use tanning beds or sun lamps.
- Live (or once lived) in an area that gets intense sunlight, Colorado included.
What Our Patients Say
“Was diagnosed with a melanoma spot on my back. Dr. Tweed did my surgery in July and so far all is good. Just went this week for my 3 month check-up and still good. Dr. Tweed is wonderful!” – Terri W.
Common Types of Skin Cancer
- Basal Cell Carcinoma
- Squamous Cell Carcinoma
- Melanoma
What is Basal Cell Carcinoma (BCC)?
Basal cell carcinoma (BCC) is the most common form of skin cancer. More than two million cases of this skin cancer are diagnosed in the United States each year.
What Does Basal Cell Carcinoma Look Like?

Often the only sign of BCC is a growth, which can vary in size from a few millimeters to several centimeters in diameter. It often appears as a shiny bump, raised pink or red spot or a sore that won’t heal.
BCCs may look like a sore that:
- Bleeds easily
- Won’t heal, or heals and returns
- Oozes or crusts over
- Has a sunken center, like a crater
- Has visible blood vessels in or around it
Basal Cell Carcinoma Treatment
Depending on how severe the BCC is and how far it has spread, your doctor will discuss options for treatment with you.
- Medicated creams and minor surgery: Creams that contain a drug, such as imiquimod or 5-fluorouracil, can be used to treat early BCC. A minor surgical procedure can be used to remove the cancer if it is beyond being treated with a cream.
- Mohs Surgery: For more aggressive lesions or those in cosmetically important areas (such as the face, ears, etc) Mohs Micrographic Surgery is performed.
What is Squamous Cell Carcinoma (SCC)?
SCC is the second most dangerous type of skin cancer and it is fast growing. This skin cancer tends to develop on skin that has been exposed to the sun over many years and therefore, occurs on sun-exposed areas of the skin. However, it is also possible to get SCC on any part of the body, including the inside of the mouth, lips, and genitals. According to the AAD, People who use tanning beds have a much higher risk of getting SCC. They also tend to get SCC earlier in life.
What Does Squamous Cell Carcinoma Look Like?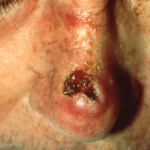
SCC can vary in appearance from a raised lesion with a thick stuck-on scale to a growing open, non-healing sore. If left untreated, squamous cell carcinomas run the risk of spreading to other parts of the body.
Causes Of Squamous Cell Carcinoma
- UV exposure is the #1 cause of SCC
- Lengthy exposure to cancer-causing chemicals
- Tobacco Use
Squamous Cell Carcinoma Treatment
Prompt treatment, often utilizing the Mohs surgery technique, allows removal while preserving as much normal surrounding skin as possible. Here are the possible treatment options you can discuss with your doctor:
- Excision
- Mohs surgery
- Radiation
When the SCC is caught early, it may be treated by curettage and electrodesiccation, photodynamic therapy or laser treatment.
What is Melanoma?
Melanoma is the deadliest type of skin cancer. When found early and treated, the cure rate is nearly 100%. At the Forefront Dermatology, formerly Asarch Dermatology, we are dedicated to early detection and Melanoma research to cure this deadly skin cancer.
Melanoma grows from pigment cells (melanocytes) in the outer layer of the skin (epidermis). Melanomas usually start as a skin lesion and tend to spread out within the epidermis before moving into the deeper layer of the skin (the dermis).
What Causes Melanoma?
As many as 90% of melanomas are estimated to be caused by UV exposure. In its early stages, melanoma can be successfully removed and monitored by regular skin screenings. In fact, survival rates can exceed 90-95% inearly-stagee melanoma.
Prevention, protection and early detection are absolutely essential.
- Prevention means limiting exposure to UV radiation. This includes UV from sunlight and artificial sources, such as tanning beds.
- Protection means wearing sun protective clothing and a broadband sunscreen with an SPF of 30 or higher, while also seeking shade when possible.
- Early detection means doing self-screenings and visiting your doctor for your annual skin check.
Who Can Get Melanoma?
Melanoma can occur in adults of any age. Anyone can get it. Early detection is key, so it is important to take time to look at the moles on your skin. When checking your skin, you should know the signs and symptoms of melanoma.
What Does Melanoma Look Like?
Melanoma lesions are unevenly shaped with irregular borders and can be multi-colored, though they are often brown or black.
The most common early signs of melanoma are:
- A mole that is growing
- An unusual looking mole (one that does not look like any other mole on your skin)
- A mole with an uneven border, blurred border, odd shape and different colors
Symptoms of Melanoma
In the early stages, melanoma may not cause any symptoms, however, you may develop:
- Itching
- Bleeding
- Pain
DiagnosING Melanoma
These characteristics are used by dermatologists to classify melanomas. Look for these signs: asymmetry, irregular borders, more than one or uneven distribution of color, or a large (greater than 6mm) Diameter. Finally, pay attention to the evolution of your moles – know what’s normal for your skin and check it regularly for changes.
The evolution of your mole(s) has become the most important factor to consider when it comes to diagnosing a melanoma. If you see one or more of these signs, make an appointment with your dermatologist immediately.
The first signs can appear in one or more atypical moles and not all melanomas fall within the ABCDE melanoma guidelines. All suspicious moles or lesions should be brought to the attention of your dermatologist immediately.
- A – Asymmetrical Shape – Melanoma lesions are often irregular, or not symmetrical, in shape. Benign moles are usually symmetrical.
- B – Border – Typically, non-cancerous moles have smooth, even borders. Melanoma lesions usually have irregular borders that are difficult to define.
- C – Color – The presence of more than one color (blue, black, brown, tan, etc.) or the uneven distribution of color can sometimes be a warning sign of melanoma. Benign moles are usually a single shade of brown or tan.
- D – Diameter – Melanoma lesions are often greater than 6 millimeters in diameter (approximately the size of a pencil eraser).
Melanoma Treatment
These are examples of the types of treatment available for melanoma. Based on your personal history, pathology report, and stage at diagnosis, your doctor may recommend one or more of the following:
- Surgery – Surgery is the mainstay of therapy for early-stage melanoma and for the resection of an isolated metastatic melanoma site. There are several different types of surgeries.
- Clinical Trials – Clinical trials are research studies to test promising new or experimental cancer treatments. There are hundreds of clinical trials happening at any given time, and most experts agree that for a late-stage diagnosis, clinical trials are the best treatment option.
- Immunotherapy – Immunotherapy is a type of systemic therapy used in the treatment of melanoma at high risk for recurrence and metastases.
- Targeted Therapy – Targeted therapy is a type of therapy where drugs (or other substances) “target” the abnormal aspects of tumor cells without harming normal cells. Several targeted therapies have been approved for use in treating various cancers, and this approach is now being evaluated in melanoma.
- Chemotherapy – Chemotherapy is a type of systemic therapy intended to destroy melanoma cells throughout the body. Chemotherapy has shown limited success in the treatment of melanoma. Each case is unique – your doctor will want to review your full pathology report and your medical history with you when discussing treatment, to determine the best course of action.
Surgery For Treating Melanoma
Surgery is the mainstay of therapy for early-stage melanoma and for the removal, or resection, of a diagnosed melanoma. Skin biopsy techniques and sentinel lymph node biopsies are first-line surgical procedures used in diagnosing melanoma. Once diagnosed, many other types of surgery are employed when appropriate.
The initial biopsy may be performed by a dermatologist or dermatologic surgeon. Surgery to remove melanoma may be performed by a surgical oncologist, a plastic surgeon, a head-and-neck surgeon or by a combination of these specialists, using the following techniques:
- Simple Excision: thin melanomas are removed along with a small amount of non-cancerous skin at the edges.
- Mohs Surgery: a small section of apparently normal skin beyond the visible melanoma is removed and looked at under a microscope. If abnormal cells are identified, another small section is removed and this process continues until the cells removed no longer look abnormal.
- Wide Local Excision: this excision is used to decrease the chance of local recurrence. A wide excision, usually 1-2 cm, is made around the original melanoma site, and the tissue is sent to the pathologist for evaluation.
- Sentinel Lymph Node Biopsy: a radioactive tracer and dye are injected into the site of the primary melanoma to “drain” the lymph node basin. They are then examined under a microscope to determine if there are any melanoma cells detected.
Dr. Asarch’s Experience in Treating Melanoma
Dr. Richard Asarch, M.D., founder of the Forefront Dermatology, formerly Asarch Dermatology Skin Rejuvenation and Associate Clinical Professor of Dermatology at the University Of Colorado School Of Medicine with the MRF’s Humanitarian Award.
The Melanoma Research Foundation (MRF) is the largest independent non-profit organization devoted to melanoma. Committed to the support of medical research in finding effective treatments and eventually a cure for melanoma, the MRF also educates patients, caregivers and physicians about the prevention, diagnosis and treatment of melanoma.
The MRF is also an active advocate for the melanoma community, helping to raise awareness of this disease and the need for a cure. At the Forefront Dermatology, formerly Asarch Dermatology, we strongly support this effort.
Less Common Types of Skin Cancer
- Merkel cell carcinoma (MCC) – This skin cancer is rare. It is also aggressive. If you have been diagnosed with MCC, find a doctor who has experience treating it.
- Dermatofibrosarcoma protuberans (DFSP) – DFSP grows slowly and rarely spreads. Treatment is important because DFSP can grow so deep it reaches the bone.
What Is Dermatofibrosarcoma Protuberans (DSFP)?
Dermatofibrosarcoma Protuberans (DSFP) is a rare skin cancer that can spread if not treated. The exact cause of DSFP is still unknown, though occurrences in skin that has been badly injured, such as a burn, seem to be more common than on otherwise healthy skin. Anyone can get DSFP at any age, though most cases are diagnosed between age 20 and 50.
DSFP begins in the dermis, the middle layer of the skin and tends to grow slowly. It may first appear as a lump under the skin and turn into a raised, pigmented patch on the surface. In children, you may think it is a birthmark. This type of skin cancer is rare and tends to grow slowly. It has a high survival rate and rarely spreads when treated. Without treatment, DFSP can grow into the fat, muscle tissue and even the bones making treatment very difficult.
Most treatment plans include surgery to remove the cancer. If DFSP has progressed deeper into the muscle or bone, other treatment may be necessary. A treatment plan for DFSP usually includes either excision or Mohs Surgery.
Schedule a Consultation
If you have noticed any of the above symptoms of skin cancer, contact Forefront Dermatology, formerly Asarch Dermatology. Call us at 303-761-7797 to schedule an appointment. Our practice serves Englewood, Lakewood, Castle Rock, and surrounding areas.
